Dr. Joel Kopelman, a leading facial plastic and oculoplastic surgeon at Kopelman Aesthetic Surgery in New York City, has over 35 years of experience with eyelid surgery. Knowing lower blepharoplasty anatomy is key to safe and natural results. This guide explains the main layers and landmarks of the lower eyelid and how they guide surgery.
Lower blepharoplasty anatomy includes the skin, muscles, ligaments, and fat pads that shape and protect the eyelid. A careful study of these details allows Dr. Kopelman to refresh the eye area while protecting eye health.
Key Takeaways
- Lower blepharoplasty anatomy covers skin, muscles, fat pads, and support ligaments of the lower lid.
- Accurate knowledge of eyelid measurements helps plan safe incisions and protect nerves.
- Surgeons choose between transconjunctival or transcutaneous approaches based on skin and fat.
- Good planning, careful incisions, and follow-up care reduce swelling, scars, and rare risks.
- Dr. Joel Kopelman’s extensive experience ensures natural-looking results and long-lasting eyelid support.
Lower Eyelid Aging Stages and Early Signs
Aging of the lower eyelid starts before most people notice changes. Early changes include small fat shifts and mild loose skin that cause faint shadows. Later, fat pads bulge and fine lines appear as the septum weakens. In advanced stages, ligaments loosen and deeper hollows form. Knowing these stages helps patients decide when to seek treatment.
Table of Contents
ToggleDr. Joel Kopelman’s Credentials
Dr. Kopelman is double board-certified in facial plastic and oculoplastic surgery. He has written in medical journals and taught other doctors. His background ensures the information here is accurate and based on current best practices.
Importance of Surgeon Experience
Lower blepharoplasty is a delicate surgery that requires years of training. The eyelid contains nerves, muscles, and small vessels that must be protected at every step.
Choosing a surgeon with extensive experience, like Dr. Joel Kopelman, reduces the risk of complications and improves both safety and appearance. Highlighting experience builds trust and supports the article’s credibility.
Anatomy of the Lower Eyelid
The lower eyelid has several layers that protect the eye and give shape to the lid. Each layer must be understood before surgery.
Key Anatomical Measurements
Surgeons use precise measurements to avoid harm. The capsulopalpebral fascia fuses with the orbital septum about 4–5 mm below the lower tarsal border. The lacrimal canaliculus is about 2.5 mm deep. The infraorbital nerve leaves the foramen about 8–10 mm below the orbital rim. These reference points guide safe fat removal and incision planning.
Skin and Muscle Layers
The outer layer is very thin skin. Under it is the orbicularis oculi muscle, which closes the eye and supports the lid. The pretarsal orbicularis, located just in front of the tarsal plates, gives strength and helps form the natural lower-lid fold. Deep inside, the inferior tarsal muscle adds gentle pull and keeps the lid in place. Each layer must be handled with care during surgery to avoid scars or weakness.
Role of Skin Quality in Surgical Planning
Skin thickness and sun damage affect the surgical plan. Thin skin may need less fat removal to prevent hollowing. Skin with heavy sun damage may benefit from laser resurfacing after surgery. Dr. Kopelman checks skin quality during consultation to choose the safest and most natural approach.
Orbital Septum and Fat Pads
Below the muscle is the orbital septum, a thin wall separating the eyelid from orbital fat. With age this wall weakens, letting fat pads bulge and create under-eye bags. Identifying each fat pad allows removal or repositioning for a smooth contour.
Suborbicularis Oculi Fat (SOOF)
Beneath the muscle lies the suborbicularis oculi fat soof, a deep mid-face fat pad that supports the lower eyelid and cheek. Loss or drop of this fat creates a hollow look at the lid cheek junction. Repositioning or adding volume here during surgery restores a smooth blend between eyelid and cheek.
Lower Eyelid Fat Pad Management Strategies
Managing fat pads is central to lower blepharoplasty. Instead of only removing fat, many surgeons reposition it to smooth the lid cheek junction and avoid a hollow look. Dr. Kopelman evaluates each compartment to decide whether to remove, move, or combine both methods.
Lid Cheek Junction
The lid cheek junction is where the lower eyelid meets the upper cheek. Aging and fat descent can cause a step or shadow here. Modern surgery aims to restore a soft, natural junction by adjusting fat and tightening support tissues.
Ligaments and Retractors
The lower eyelid is supported by the capsulopalpebral fascia and canthal tendons. These ligaments connect the lid to the bone and maintain movement. During surgery, the lid retractor is preserved or tightened to keep the eyelid stable and blinking normally.
Medial Canthal Tendon and Inner Corner Support
At the inner corner of the eye, the medial canthal tendon anchors the lids to the bone near the nose. This tendon keeps the eyelid edge straight and in the right place. Protecting it prevents lid droop and keeps the inner corner of the eye looking natural.
Tarsal Plates and Structural Support
The lower lid contains tarsal plates, strong tissue that gives shape and supports the eyelashes. Recognizing the plates is important to keep a natural lid contour after surgery.
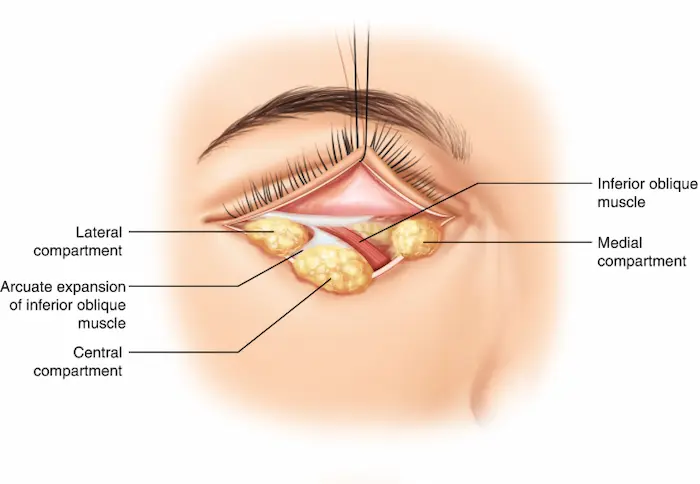
Inferior Oblique Muscle
Beneath the fat pads is the inferior oblique muscle, which helps move the eye and stabilize the lower lid. Protecting this muscle during surgery avoids double vision or movement problems.
Arcuate Expansion and Arcus Marginalis
Near the orbital rim, the arcuate expansion of the orbital septum blends with the arcus marginalis, a fibrous band that attaches the septum to bone. These structures mark the border between eyelid and cheek and guide fat repositioning to correct tear-trough deformities.
Lockwood Ligament and Eyelid Suspension
Deep in the orbital floor lies the lockwood ligament, also called the suspensory ligament of the globe. It supports the eyeball and influences lower lid position. Surgeons protect this ligament to maintain natural eye support.
Surgical Relevance of Anatomy
Knowing these layers is essential for planning and safety.
Key Landmarks and Risk Areas
Important landmarks include the infraorbital rim, tear trough, and lateral canthus. These guide incision placement and fat removal. Surgeons avoid the infraorbital nerve and small blood vessels to reduce the risk of numbness or bruising. Many patients ask if lower blepharoplasty is dangerous, and Dr. Kopelman explains how careful planning keeps the procedure safe.
Protecting Nerves and Vessels
The infraorbital nerve gives feeling to the cheek and upper lip. Careful dissection along the septum and fat pads prevents nerve damage and reduces bruising.
Operative Pearls for Surgeons
Surgeons often use blunt dissection to follow the septum and locate fat compartments. A lateral canthopexy may be added if the lid is loose to keep it in the right position. Fat can be moved over the infraorbital rim to soften the tear trough and avoid hollows. These details show why an experienced surgeon is important.
Lower Blepharoplasty Technique
Lower blepharoplasty can be performed through various approaches, depending on the skin quality, amount of fat, and patient goals.
Transconjunctival vs Transcutaneous Approaches
The transconjunctival approach uses an incision inside the lower lid to remove or move fat without an outside scar. It works well for younger patients with little extra skin.
The transcutaneous approach makes a small cut below the lashes to tighten skin and fat. It is suitable for patients with loose skin or muscle. Dr. Kopelman selects the method after full evaluation.
Choosing the Right Surgical Technique
Selecting the correct surgical technique is key for a safe and natural outcome.
Dr. Kopelman reviews each patient’s eyelid support, skin quality, and fat distribution before choosing the best method. Some patients require only fat repositioning, while others benefit from skin tightening or a combination of approaches.
Explaining these choices helps patients understand why every plan is unique. Learn more about the types of eyelid surgery to see how each approach fits different needs.
Comparing Surgical Techniques and Outcomes
Different lower blepharoplasty methods can give different results.
The transconjunctival approach is most effective when there is minimal extra skin and primarily fat bulging. The transcutaneous approach is more suitable when the skin and muscle are loose and require tightening.
Dr. Kopelman explains each surgical technique during consultation so patients understand healing times, scars, and expected results.
Lower Lid Blepharoplasty Incision
Incisions vary by approach. Transconjunctival cuts hide inside the lid. Transcutaneous cuts lie along the lash line and fade over time. Proper placement gives the best cosmetic result.
Anesthesia, Scars, and Recovery
Lower Blepharoplasty Anesthesia
Most surgeries use local anesthesia with sedation. This keeps patients comfortable while minimizing the risks associated with general anesthesia. Dr. Kopelman explains all options during the consultation.
Pain Management and Comfort
Is eyelid surgery painful? Pain is usually mild and managed with over-the-counter medicine and cold compresses. Patients keep their head raised and use gentle icing to limit swelling.
Lower Blepharoplasty Scars
A transcutaneous approach leaves a fine scar hidden in the natural crease. The transconjunctival method leaves no external scar. Good wound care and sun protection help scars heal well.
Early Recognition and Management of Complications
Serious problems are rare, but they must be treated promptly. Sudden pain, vision change, or fast swelling may signal a retrobulbar hematoma. Patients get clear instructions on when to call the office or seek emergency care.
Postoperative Follow-Up
Follow-up visits allow Dr. Kopelman to monitor the healing process. A first visit is done within a few days, followed by visits at one week, one month, and three months. These checks ensure safe recovery.
Recovery Milestones Week by Week
Knowing what to expect each week helps patients feel calm and prepared.
- Week 1: Most swelling and bruising peak in the first two days and then slowly fade.
- Week 2: Stitches, if present, are removed, and normal activities can resume.
- Week 3–4: Most swelling is gone, and the final contour begins to show.
- Month 3: Scars continue to fade and eyelids settle into their long-term shape.


This timeline reassures patients and sets realistic expectations.
Pre-Operative Preparation and Recovery Timeline
Preparation includes stopping certain medicines, quitting smoking, and having health checks. Swelling and bruising usually last one to two weeks. Most patients return to normal activity after 10–14 days.
Preparing Your Home for Recovery
A smooth recovery starts before the surgery date. Patients can stock cold compresses, extra pillows for head elevation, and easy-to-cook meals.
Arrange for a friend or family member to drive you home and help during the first day. These simple steps reduce stress and support safe healing.
Patient Lifestyle Tips for Better Healing
Healthy habits improve healing. Eat a balanced diet with protein and vitamins C and K, drink enough water, and avoid alcohol. Keep blood pressure steady and follow all instructions.
Lifestyle Factors That Affect Results
Long-term results depend on more than surgery alone. Sun exposure, smoking, and poor sleep can speed up skin aging and shorten the benefits of blepharoplasty.
Patients who maintain healthy habits—such as wearing sunscreen, avoiding tobacco, and sleeping well—help protect their investment and keep the eyelids looking fresh.
Patient Education and Informed Consent
Each patient receives clear explanations of expected results, risks, and other treatment choices. Detailed counseling builds trust and helps patients feel confident in their decision.
Advances in Lower Blepharoplasty Technology
New tools improve precision and safety. High-frequency cautery controls bleeding with little tissue damage. Modern sutures support wounds and speed healing. Some cases use platelet-rich plasma to reduce swelling and promote recovery.
Cost Factors and Insurance
Costs vary by technique, anesthesia, and combined procedures; the typical price range is $8,500 to $10,000. And, because this surgery is usually cosmetic, insurance rarely covers it unless drooping skin blocks vision.
Common Complications and Management
Temporary swelling, bruising, or dryness may occur. Rare problems, such as lid malposition or infection, are minimized through careful technique and follow-up care. For more information on conditions that can affect the lids, visit our guide on eyelid problems.
Key Takeaways for Patients and Surgeons
Lower blepharoplasty anatomy includes skin, muscles, orbital septum, fat pads, and key ligaments. Knowing these parts allows safe incisions, nerve protection, and natural results.
At Kopelman Aesthetic Surgery, Dr. Joel Kopelman combines decades of experience with a deep knowledge of the anatomy of lower blepharoplasty to create lasting, natural rejuvenation.
Key Questions to Ask During Consultation
Before booking surgery, patients should prepare a short list of questions.
Helpful examples include:
- Which surgical technique is best for my eyelid type?
- How much swelling and bruising should I expect?
- What are the risks to eye health or vision?
- How many lower blepharoplasty procedures have you performed?
Asking these questions helps patients understand the plan and feel confident about their care.
Ideal Candidates for Lower Blepharoplasty
This surgery is suitable for adults with lower eyelid bags, fat pad bulges, or loose skin who are in good health. Candidates often report constant under-eye bags despite rest or creams. Dr. Kopelman reviews health history, tear production, and lid support to confirm safety.
Combination Procedures for Full Rejuvenation
Lower blepharoplasty may be combined with fat grafting, midface lifting, or skin resurfacing for a balanced result. Combining treatments allows for a single recovery period and a more comprehensive refresh.
Non-Surgical Alternatives
People with mild concerns may opt for non-surgical options. Fillers, laser resurfacing, or skin-tightening devices can reduce shadows and fine lines with little downtime. These treatments can delay surgery for some patients.
Protecting Eye Function After Surgery
Eye comfort and function are just as important as cosmetic results. Patients should watch for signs of dry eye, light sensitivity, or blurred vision.
Regular eye exams and follow-up visits allow Dr. Kopelman to check tear production, lid position, and corneal health. Early care keeps eyes healthy, and the results are long-lasting.
Imaging and Diagnostic Evaluation
Modern imaging gives precise views of eyelid anatomy. High-resolution photos and digital morphing show before-and-after comparisons. MRI or CT scans may be used to spot hidden fat or structural problems.
Role of Pre-operative Imaging
Pre-operative imaging gives a detailed map of the lower eyelid and surrounding bone. High-resolution photos, CT scans, or MRIs help detect hidden fat pockets, weak ligaments, or asymmetry.
These studies allow Dr. Kopelman to plan the incision and fat management with greater accuracy and safety. Better planning means fewer surprises during surgery and more predictable results.
Use of 3D Photography for Planning
Three-dimensional photos let surgeons analyze contour, fat distribution, and symmetry. Dr. Kopelman uses these images to plan surgery and explain likely results. This technology enables patients to visualize realistic outcomes.
Eyelid Anatomy in Different Ethnic Groups
Lower eyelid anatomy is not the same for everyone. Ethnic background can influence skin thickness, fat distribution, ligament strength, and eyelid shape.
These differences guide the surgical technique and enable the surgeon to plan a natural-looking result:
- East Asian patients often have a thicker orbital septum and stronger attachment of the arcus marginalis. Fat pads may sit slightly lower, and the lid crease can be less defined.
- Mediterranean and Middle Eastern patients may show more prominent fat pads and thicker skin, which can require stronger tightening of the orbicularis or septum.
- African and African American patients often have thicker, more elastic skin that resists fine wrinkling but can form noticeable scars if not handled with care.
- Northern European patients usually have thinner skin and weaker ligament support, which increases the chance of early fat herniation and visible hollows.
Dr. Kopelman evaluates these differences during the consultation. He adjusts incision placement, fat management, and tension of the medial canthal tendon to match each patient’s unique features.
For Surgeons: Quick Reference Summary
- Septum Fusion Point: about 4–5 mm below the lower tarsal border.
- Lacrimal Canaliculus Depth: about 2.5 mm vertical segment.
- Infraorbital Nerve Position: about 8–10 mm below the orbital rim.
- Preferred Approaches: Transconjunctival for minimal skin excess; transcutaneous when skin or muscle tightening is needed.
Long-Term Outcome Studies and Evidence
Research shows that lower blepharoplasty gives lasting improvement in eyelid contour for many years. Studies report high patient satisfaction and low complication rates when performed by skilled surgeons.
Frequently Asked Questions
+ How long do results last?
Results can last for many years. Fat that is removed or moved rarely comes back, though natural aging continues.
+ Can this surgery be done with upper eyelid surgery?
Yes. Dr. Kopelman often treats upper and lower lids in the same visit for a balanced look and a single recovery period.
+ Is the surgery painful?
Pain is usually mild. Local anesthesia with sedation keeps you comfortable. Simple pain medicine controls any soreness in the first few days.
+ When can I return to normal activities?
Most people return to daily routines in about 10 to 14 days. Mild swelling or bruising may last a little longer.
+ Will I have visible scars?
A transconjunctival approach leaves no outside scar. A transcutaneous approach leaves a fine line along the lash line that fades with time.
Next Steps
Lower blepharoplasty is a precise procedure that relies on a careful surgical technique and a full understanding of eyelid anatomy. Dr. Joel Kopelman uses advanced methods to remove or reposition fat, tighten skin, and protect delicate eye structures.
If you are ready to explore your options, schedule a consultation with Kopelman Aesthetic Surgery in New York City. During your visit, Dr. Kopelman will explain the surgical technique in simple terms, answer questions, and create a plan tailored to your needs.